Dr. Tanmay Srivastava
Temporomandibular joint disorder (TMD) is a common condition affecting the temporomandibular joint (TMJ), which connects the jawbone to the skull. Among the various manifestations of TMD, degenerative condylar change is a significant aspect that contributes to the pathology and symptoms. In this article, we will explore the degenerative condylar change in TMD, its underlying causes, and its impact on patients.
Degenerative condylar change refers to the progressive deterioration of the condylar portion of the TMJ, which is responsible for the jaw's movement. This degeneration involves structural and functional alterations, leading to pain, restricted jaw movement, and other related symptoms. The exact mechanisms behind the development of degenerative condylar change are not fully understood, but several factors are believed to contribute to its occurrence.
One of the primary causes of degenerative condylar change is excessive or abnormal joint loading. This can result from various factors such as bruxism (teeth grinding), malocclusion (improper alignment of the teeth), trauma to the jaw, or habitual behaviors like nail biting or chewing gum excessively. The repeated or prolonged mechanical stress on the TMJ can lead to wear and tear of the condylar cartilage, causing degenerative changes over time.
Another factor that may contribute to degenerative condylar change is inflammation. Inflammatory conditions like arthritis or synovitis can affect the TMJ, leading to cartilage degradation, bone remodeling, and subsequent degeneration of the condyle. Additionally, certain systemic conditions such as rheumatoid arthritis or osteoarthritis may also contribute to the development of degenerative changes in the TMJ.
The consequences of degenerative condylar change can significantly impact patients' quality of life. Patients may experience pain or discomfort in the jaw joint, which can radiate to the face, ear, or neck. Jaw movement may become limited, leading to difficulties in eating, speaking, and performing daily activities. Clicking, popping, or grating sensations during jaw movement may also be present. In severe cases, degenerative condylar change can result in joint dysfunction, leading to malocclusion, facial asymmetry, and even changes in bite alignment.
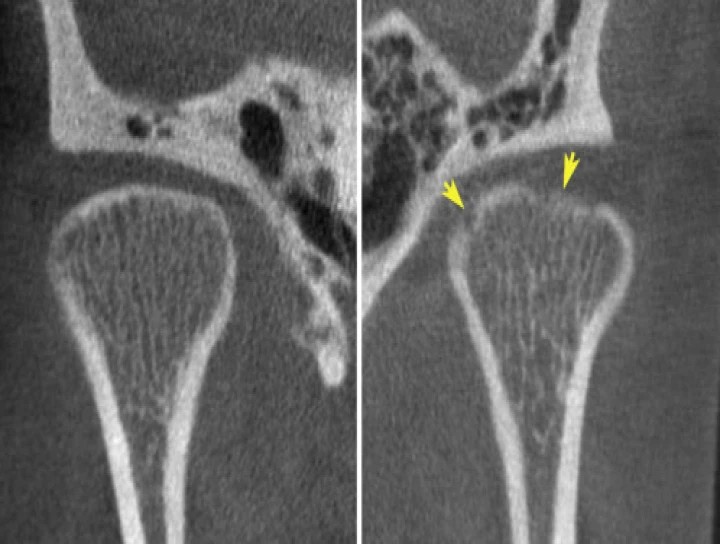
Diagnosing degenerative condylar change in TMD typically involves a thorough clinical evaluation, including medical history, physical examination, and imaging studies such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans. These diagnostic tools help assess the extent of condylar changes, evaluate joint alignment, and identify any associated abnormalities.
Treatment approaches for degenerative condylar change in TMD aim to alleviate pain, improve jaw function, and slow down or halt the progression of degeneration. Conservative measures may include lifestyle modifications (e.g., stress reduction techniques, avoiding excessive jaw movements), physical therapy, and the use of oral appliances to provide joint support and reduce clenching or grinding. In some cases, medication such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may be prescribed to manage pain and inflammation.
For more severe cases or when conservative measures fail to provide relief, surgical interventions may be considered. Surgical options range from arthroscopy (minimally invasive joint exploration and repair) to open joint surgery, which involves more extensive procedures like joint reconstruction or replacement.
In conclusion, degenerative condylar change in TMD is a significant aspect of the disorder, characterized by progressive deterioration of the condylar portion of the TMJ. Excessive joint loading and inflammation are among the key factors contributing to this degeneration. The resulting symptoms can significantly impact patients' daily lives, causing pain, restricted jaw movement, and functional limitations.


No Any Replies to “The Degenerative Condylar Change in Temporomandibular Joint Disorder.”
Leave a Reply