Endodontic surgery involves surgical procedures to save a tooth that cannot be saved by nonsurgical root canal treatment. It involves various procedures like Abscess drainage, Corrective Surgery, Intentional re-implantation and the most common, Periapical Surgery.
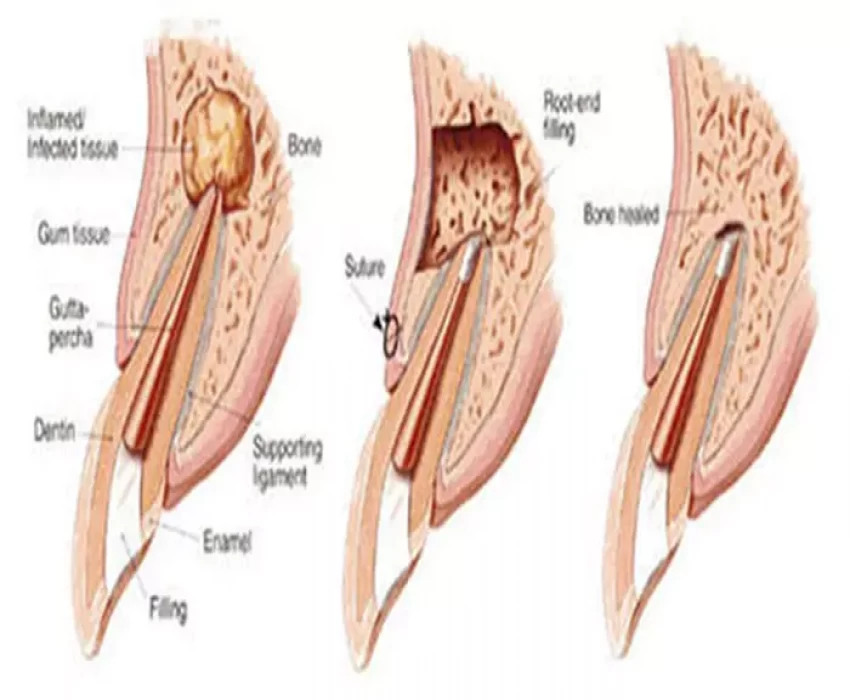
The main goal of apical surgery is to prevent bacterial leakage from the root-canal system into the periradicular tissues by placing a tight root-end filling following root-end resection. Clinicians are advised to utilize a surgical microscope to perform apical surgery to benefit from magnification and illumination. In addition, the application of microsurgical techniques in apical surgery, i.e., gentle incision and flap elevation, production of a small osteotomy, and the use of sonic- or ultrasonic driven microtips, will result in less trauma to the patient and faster postsurgical healing. A major step in apical surgery is to identify possible leakage areas at the cut root face and subsequently to ensure adequate root-end filling. Only a tight and persistent apical obturation will allow periapical healing with good longterm prognosis. The present paper describes current indications, techniques and outcome of apical surgery.
Introduction :
Apical surgery belongs to the field of endodontic surgery that also includes incision and drainage, closure of perforations, and root or tooth resections. The objective of apical surgery is to surgically maintain a tooth that has an endodontic lesion which cannot be resolved by conventional endodontic (re-)treatment. Apical surgery has greatly benefited from continuing development and introduction of new diagnostic tools, surgical instruments and materials, making this method of tooth maintenance more predictable. Success rates approaching 90% or above have been documented in several clinical studies.
Indications
(1) Radiological findings of apical periodontitis and/or symptoms associated with an obstructed canal (the obstruction proved not to be removable, displacement did not seem feasible or the risk of damage was too great).
(2) Extruded material with clinical or radiological findings of apical periodontitis and/or symptoms continuing over a prolonged period.
(3) Persisting or emerging disease following root-canal treatment when root canal re-treatment is inappropriate.
(4) Perforation of the root or the floor of the pulp chamber and where it is impossible to treat from within the pulp cavity.
Procedure:
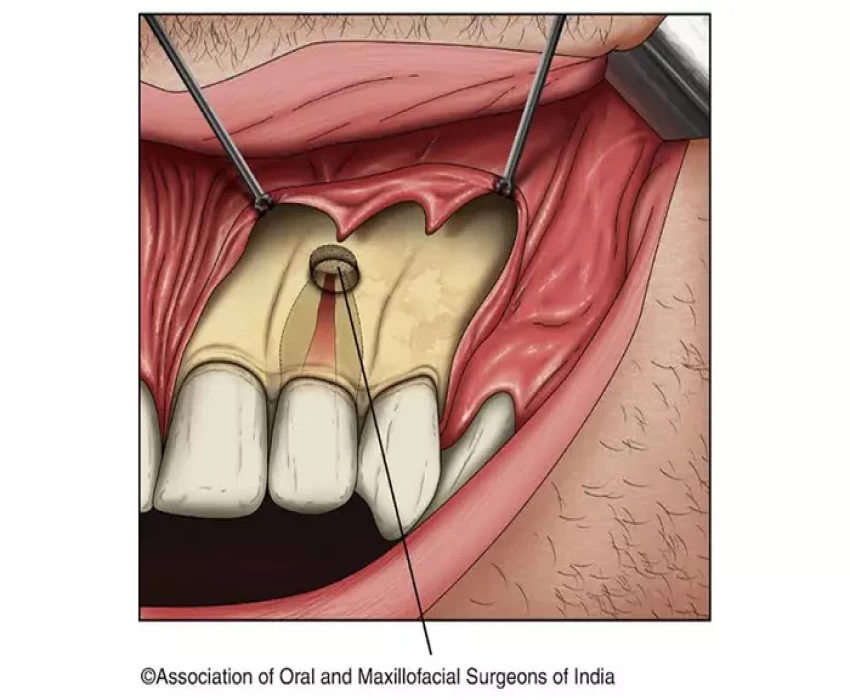
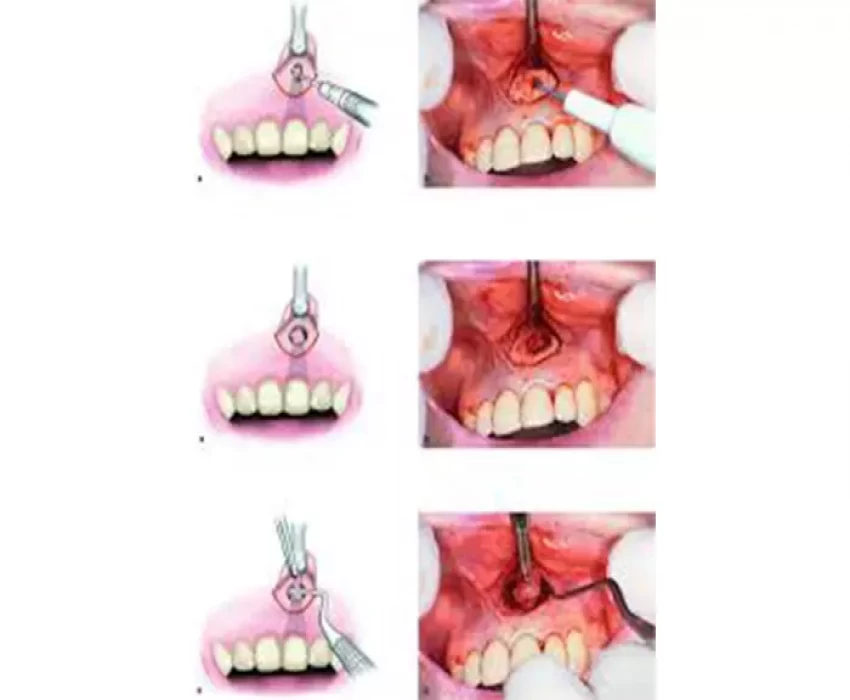
1. Reflection of Mucoperiosteal Flap.
2. Exposure of Periapical Pathology and Root Tip.
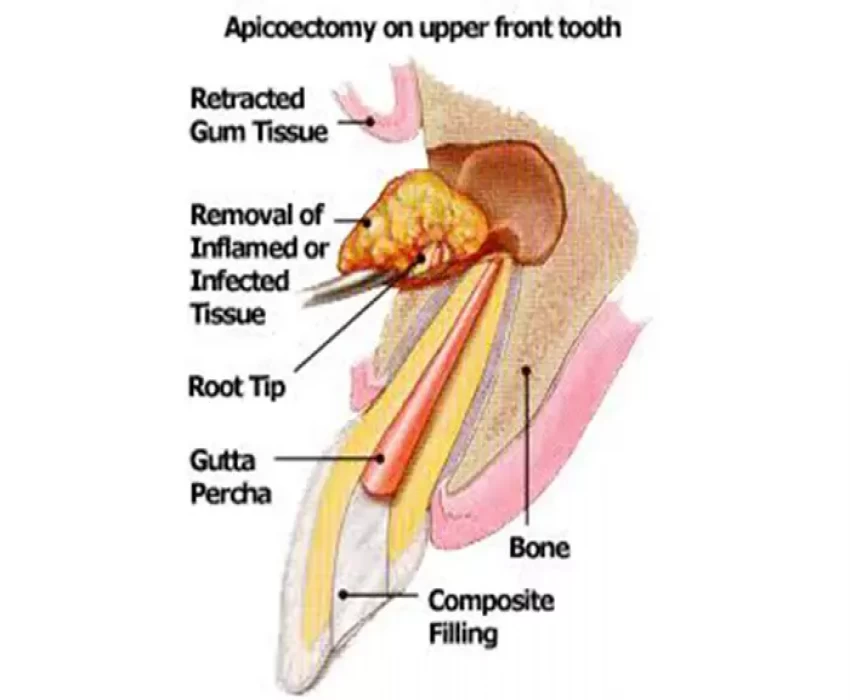
3. Removal of Periapical pathology.
4. Ressection of Root Apex
Contraindications:
For apical surgery include the following: the tooth has no function (no antagonist, no strategic importance serving as a pillar for a fixed prosthesis), the tooth cannot be restored, the tooth has inadequate periodontal support, or the tooth has a vertical root fracture. Additional general contraindications may be an uncooperative patient or a patient with a compromised medical history for an oral surgical intervention.
Outcome after apical surgery:
From a practical point of view, healing is normally evaluated 1-year post surgery, although small (<5 mm) periapical defects might heal within a few months.
Clinical healing is based on the absence of signs and symptoms such as pain, sinus tract, swelling, apicomarginal communication, and tenderness to palpation or percussion. With regard to the outcome of apical surgery, inconsistent success rates ranging from 44% to 90% were reported prior to the introduction of microsurgical techniques.
Another important issue to consider in the healing outcome of apical surgery is the difficulties and challenges of combined endo-perio lesions, in particular the absence of the buccal bone plate with a completely exposed buccal root surface