Primary Tuberculosis of the Maxillary Sinus
Tuberculosis (TB) is a chronic granulomatous infection caused by Mycobacterium tuberculosis, primarily affecting the lungs. However, extrapulmonary tuberculosis accounts for a significant proportion of cases, involving sites such as lymph nodes, bones, joints, and the genitourinary system. Involvement of the paranasal sinuses is extremely rare, with the maxillary sinus being the most commonly affected among them. Primary tuberculosis of the maxillary sinus, occurring without evidence of pulmonary or systemic TB, is an unusual clinical entity and poses a diagnostic challenge due to its nonspecific presentation.
The maxillary sinus is relatively resistant to tuberculous infection because of its well-ventilated environment, ciliary action, and bactericidal properties of sinus secretions. Primary infection is believed to occur through direct inoculation of bacilli via the nasal cavity or oral cavity, possibly following dental extraction, oroantral communication, or mucosal trauma. Hematogenous spread is another proposed mechanism, although it is more commonly associated with secondary involvement.
Clinically, primary tuberculosis of the maxillary sinus often mimics chronic maxillary sinusitis. Patients typically present with unilateral nasal obstruction, facial pain or swelling, purulent or blood-stained nasal discharge, postnasal drip, and occasionally epistaxis. Constitutional symptoms such as fever, weight loss, and night sweats may be absent, further complicating diagnosis. In some cases, intraoral manifestations such as gingival swelling, non-healing extraction sockets, or oroantral fistula may be observed.
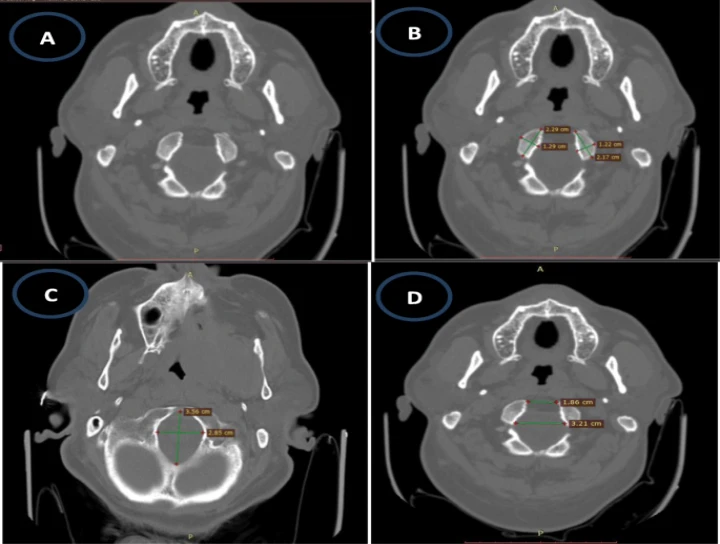
Radiographically, imaging findings are nonspecific. Conventional radiographs may show diffuse or localized opacification of the maxillary sinus. Computed tomography (CT) or cone-beam computed tomography (CBCT) provides better delineation, revealing mucosal thickening, sinus opacification, and in advanced cases, bony erosion of the sinus walls. However, these features can resemble fungal sinusitis, malignancy, or chronic bacterial infections, necessitating further investigation.
Definitive diagnosis relies on histopathological and microbiological examination. Biopsy of the sinus lining typically reveals granulomatous inflammation with epithelioid cells, Langhans giant cells, and caseous necrosis. Demonstration of acid-fast bacilli on Ziehl–Neelsen staining or detection of Mycobacterium tuberculosis by culture or molecular methods confirms the diagnosis. A thorough systemic evaluation is essential to exclude pulmonary or other extrapulmonary TB, thereby establishing the primary nature of the lesion.
Management of primary tuberculosis of the maxillary sinus primarily involves antitubercular therapy (ATT) following standard national or WHO guidelines. Surgical intervention is generally limited to diagnostic biopsy or drainage in cases with significant obstruction or secondary infection. With appropriate and timely treatment, the prognosis is favorable, and complete resolution is commonly achieved.
In conclusion, primary tuberculosis of the maxillary sinus is a rare but important differential diagnosis in patients with chronic unilateral maxillary sinus disease unresponsive to conventional therapy. Awareness of this entity, along with a high index of suspicion and multidisciplinary approach, is crucial for early diagnosis and effective management, thereby preventing unnecessary surgical interventions and potential complications.


No Any Replies to “Primary Tuberculosis of Maxillary Sinus”
Leave a Reply