Assessment of Articular Disc with MRI in Patients with Disc Displacement of the Temporomandibular Joint – MRI: The Game Changer
Temporomandibular joint (TMJ) disorders constitute a significant cause of orofacial pain and functional impairment, with internal derangement being one of the most common conditions. Disc displacement, characterized by an abnormal positional relationship between the articular disc, mandibular condyle, and articular eminence, plays a pivotal role in TMJ dysfunction. Accurate assessment of the articular disc is essential for diagnosis, treatment planning, and prognosis. Magnetic resonance imaging (MRI) has emerged as the gold standard for evaluating soft tissue components of the TMJ, making it a true game changer in the diagnosis of disc displacement.
The articular disc is a fibrocartilaginous structure that cannot be adequately visualized using conventional radiography or computed tomography, as these modalities primarily assess osseous structures. MRI, with its superior soft tissue contrast and multiplanar capability, allows direct visualization of the disc morphology, position, and functional dynamics without ionizing radiation. This advantage makes MRI particularly valuable in TMJ evaluation.
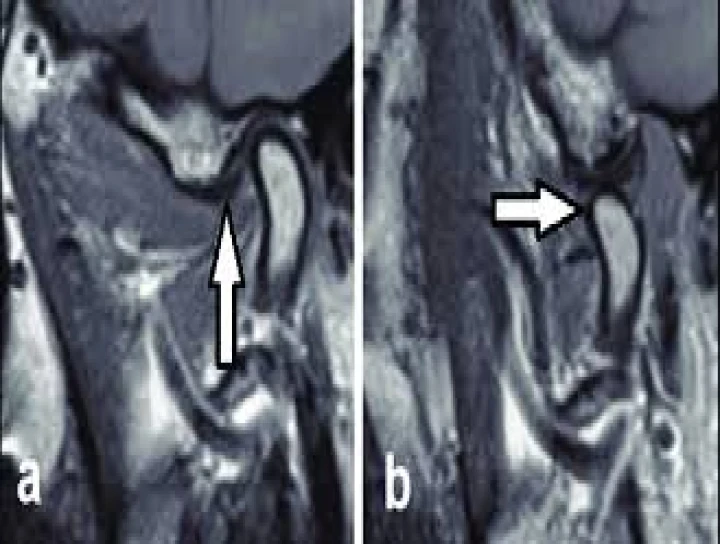
MRI enables precise identification of various types of disc displacement, most commonly anterior disc displacement with or without reduction. In the closed-mouth position, a normal disc is seen interposed between the condyle and the articular eminence, with the posterior band positioned at the 12 o’clock position relative to the condylar head. In cases of disc displacement, MRI clearly demonstrates anterior, anteromedial, or anterolateral displacement of the disc. Dynamic imaging using open- and closed-mouth views helps determine whether the disc reduces to its normal position during mouth opening, which is crucial for clinical decision-making.
Beyond disc position, MRI provides detailed information about disc morphology, including thickening, thinning, folding, or perforation, which often correlates with disease severity and chronicity. It also allows assessment of associated joint changes such as joint effusion, synovitis, bone marrow edema, and degenerative alterations of the condyle and articular eminence. These findings contribute to a comprehensive understanding of the pathophysiology of TMJ disorders.
MRI findings have a direct impact on treatment planning. Patients with disc displacement with reduction may benefit from conservative management, including occlusal splints, physiotherapy, and pharmacological therapy. In contrast, non-reducing disc displacement with structural disc deformation and inflammatory changes may require more advanced interventions such as arthrocentesis, arthroscopy, or surgical management. MRI also serves as a valuable tool for monitoring treatment outcomes and disease progression.
In addition, MRI plays a crucial role in differentiating disc displacement from other causes of TMJ pain such as inflammatory arthritis, neoplastic conditions, or developmental abnormalities. Its non-invasive nature and lack of radiation make it suitable for repeated evaluations, especially in younger patients.
In conclusion, MRI has revolutionized the assessment of the articular disc in patients with temporomandibular joint disc displacement. By providing unparalleled visualization of soft tissue structures and functional dynamics, MRI enables accurate diagnosis, guides appropriate management, and improves patient outcomes. Truly, MRI stands as a game changer in the evaluation and management of TMJ internal derangements.


No Any Replies to “Assessment of Articular Disc with MRI in Patients with Disc Displacement of Temporo-Mandibular Joint – MRI the Game Changer”
Leave a Reply