Evaluation and Management of Oral Complications in Oral Cancer Patients Undergoing Radiotherapy
Radiotherapy is a cornerstone in the management of oral cancer, either as a primary treatment modality or as an adjunct to surgery and chemotherapy. Despite its therapeutic benefits, radiotherapy to the head and neck region often results in a wide spectrum of oral complications due to the high radiosensitivity of oral tissues. These complications significantly affect patients’ quality of life and may compromise treatment compliance. Therefore, timely evaluation and effective management of oral complications are essential components of comprehensive oral cancer care.
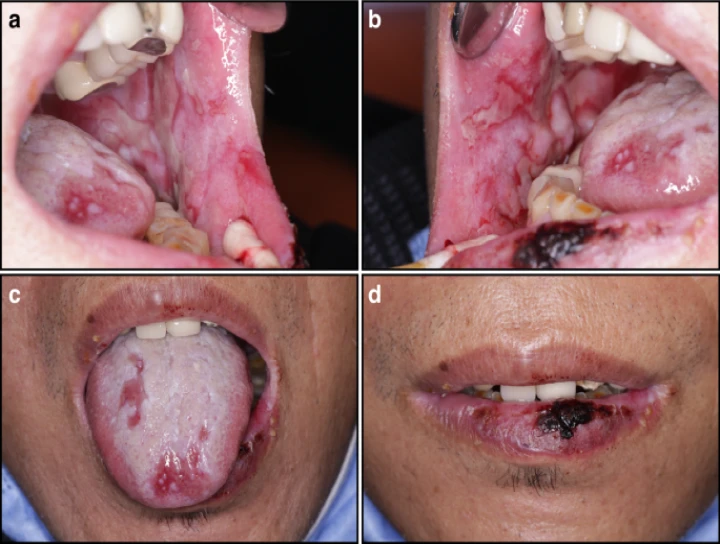
The most common acute oral complication of radiotherapy is oral mucositis, characterized by erythema, ulceration, pain, and difficulty in eating and speaking. Clinical evaluation involves grading the severity of mucositis using standardized scales such as the WHO or RTOG criteria. Management includes maintenance of meticulous oral hygiene, use of bland rinses, topical anesthetics, mucosal coating agents, and analgesics. Low-level laser therapy and cryotherapy have also shown beneficial effects in reducing the severity and duration of mucositis.
Xerostomia is another frequent and often persistent complication caused by radiation-induced damage to the salivary glands. Evaluation includes assessment of salivary flow rate and patient-reported symptoms of dry mouth. Management strategies focus on symptomatic relief through saliva substitutes, frequent water intake, sugar-free chewing gums, and sialogogues such as pilocarpine or cevimeline when appropriate. Preventive measures like intensity-modulated radiotherapy (IMRT) help reduce salivary gland damage.
Radiotherapy also predisposes patients to oral infections, particularly candidiasis, due to immunosuppression and altered oral microflora. Clinical examination and microbiological tests aid in diagnosis. Antifungal agents, both topical and systemic, along with improved oral hygiene, are essential for effective management. Dysgeusia, or altered taste sensation, is commonly reported and evaluated through patient history and taste testing. Nutritional counseling plays a vital role in managing this condition.
Late complications of radiotherapy include radiation caries, trismus, and osteoradionecrosis (ORN) of the jaws. Radiation caries is evaluated by clinical and radiographic examination and managed through topical fluoride applications, remineralizing agents, and strict dietary control. Trismus is assessed by measuring mouth opening and managed with physiotherapy, jaw exercises, and supportive appliances. Osteoradionecrosis is a serious complication requiring careful radiographic evaluation and staged management ranging from conservative therapy to surgical intervention, sometimes supplemented with hyperbaric oxygen therapy.
A multidisciplinary approach involving oncologists, oral physicians, dentists, nutritionists, and speech therapists is crucial for optimal care. Pre-radiotherapy dental evaluation, elimination of oral foci of infection, and patient education significantly reduce the severity of oral complications.
In conclusion, radiotherapy-induced oral complications are common and potentially debilitating in oral cancer patients. Early evaluation, preventive strategies, and prompt management are essential to minimize morbidity, improve quality of life, and ensure uninterrupted cancer therapy. Comprehensive oral care should be an integral part of radiotherapy protocols for oral cancer patients.


No Any Replies to “Evaluation and Management of Oral Complications in Oral Cancer Patients Undergoing Radiotherapy”
Leave a Reply